Measles Outbreak: The Risks and Challenges of Using the MMR Vaccine as Post-Exposure Prophylaxis
Show me the data! There are no clinical trials or studies to support this practice.
Child dies of measles in Lubbock, Texas
Firstly, I would like to say the death of any child is devastating no matter the circumstances. My heart goes out to the family of those child. No child’s death should be used to further any political narrative.
An unvaccinated child has died of measles, Texas officials announced Wednesday February 26, the first death from measles in the United States in a decade. The child’s death in a hospital in Lubbock, in West Texas, comes as the largest measles outbreak in the state in over 30 years is now spreading to New Mexico.
Source: https://www.dshs.texas.gov/news-alerts/texas-announces-first-death-measles-outbreak
This story lacks a great deal of information and details about the child.
This is all the news has reported:
The patient was a school-aged child
The child was allegedly unvaccinated
The child was hospitalized
The child tested positive for measles
The child died
Local public health officials are not being transparent about this child’s death.
No healthy child dies from measles.
Just as we saw during the SARS-CoV-2 pandemic, deaths among adolescents (<21 years old) all had underlying medical conditions. Like adults, children and teens with obesity, diabetes, asthma or chronic lung disease, sickle cell disease, or who are immunocompromised* can also be at increased risk for getting very sick from COVID-19.
*immunocompromised include: people who have cancer and are on chemotherapy, people who have had a solid organ transplant and are taking medication to keep their transplant, people who use some medicines for a long time, like corticosteroids, those with primary immunodeficiency.
In one study of children (ages 1-17 years old) who died of COVID-19, more than two-thirds (68%) had a medical condition (excluding COVID-19) at time of death. Of children with an underlying condition, 35% had 3 or more conditions.
We have no information on the health status of this child who was hospitalized and tested positive for measles.
Rumors surfaced that the child was admitted to the hospital with RSV and pneumonia. The child tested positive for measles after hospitalized and was subsequently administered the MMR vaccine.
Source: https://x.com/DrSyedHaider/status/1895485267634463144
Of course none of this had been confirmed nor denied by Texas public health officials.
Studies demonstrate that measles post-exposure prophylaxis (PEP) with immunoglobulin (Ig) administered within 6 days of exposure can be effective, with some studies reporting 100% effectiveness. If the above is true, why did the child receive an MMR vaccine and not intravenous Ig?
Public health has been shifting vaccines from preventatives to treatments.
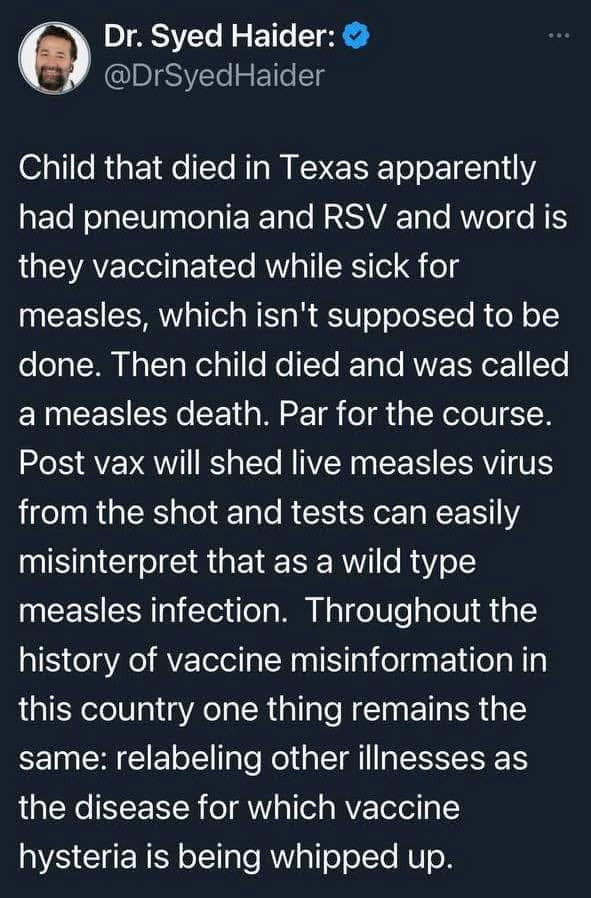
The Texas Department of State Health Services is using MMR as post-exposure prophylaxis (PEP).
“A dose of MMR is given to unvaccinated people within 72 hours of their exposure to the measles to lessen the severity of the illness if they get sick from their exposure to the virus. We are looking into if any of these cases received their MMR dose after exposure.”
There are two key concerns here.
First, where is the evidence, such as studies or clinical trials, supporting the use of the MMR vaccine as PEP?
Second, what are the potential effects of administering the MMR vaccine to someone who is already ill?
On the second point, the CDC advises against giving the MMR (measles, mumps, and rubella) vaccine to individuals who are suffering from moderate or severe illness. However, it is considered safe to administer the vaccine to those with minor illnesses, like a cold, provided they do not have a fever.
Why would medical professionals vaccinate someone who is already experiencing an illness that the vaccine is designed to prevent?
This is a very dangerous practice. They are injecting people with a live attenuated vaccine while the patient is incubating a wild-type virus. This can lead to a life-threatening cytokine storm.
World-renowned vaccinologist Dr. Geert Vanden Bossche wrote in an email “Live attenuated vaccines are notorious for causing inflammation. When infected, even mildly, it is primarily the innate immune system that is triggered, with a large production of cytokines and interleukins. This can contribute to the risk of a cytokine storm, which can be life-threatening and detrimental to generating an effective immune response. This is because high levels of inflammatory cytokines suppress adaptive immune effector cells (T cells and B cells) and skew the immune response toward Th1 response, which is more inflammatory than a balanced Th1/Th2 immune activation.”
Inoculating individuals who have active wild-type measles infections with weakened versions of the measles, mumps and rubella viruses (one dose of the MMR vaccine) can have devastating and potentially lethal consequences. In the case of the 'unvaccinated' child who tragically passed away from measles, but had RSV and pneumonia, administering the MMR vaccine, even with one dose, may have worsened the severity of their condition.
The danger of using vaccines as post-exposure prophylaxis
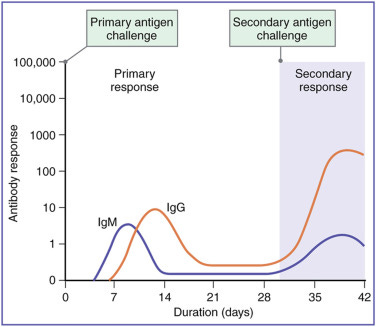
Immunity doesn't develop immediately. Antibodies don't get produced right away, it takes at minimum 7 to 10 days after injection or infection for antibodies to begin to be produced. According to the CDCs own web page explaining how vaccines work, because immunity can take weeks to develop after vaccination, it is possible to become infected in the weeks immediately following vaccination. Protective immune responses that are specifically tailored to prevent infectious diseases take longer to generate.
I scanned the literature and could not find any published studies on the use of the MMR as post-exposure prophylaxis. The only references I found cite the CDC website. If you're aware of any, please share the link in the comments.
Dr. Geert Vanden Bossche provided an example of a trial conducted in West Africa using Merck’s live vector Ebola vaccine. This trial aimed to test the vaccine efficacy and effectiveness during outbreaks using ring vaccination as a novel cluster-randomized trial design. Ring vaccination is defined as the vaccination of a cluster of individuals at high risk of infection, owing to their social or geographical connection to a confirmed index case.
There were 7,651 contacts randomized into one of two groups: i) immediate vaccination with rVSV-ZEBOV or ii) the same vaccination but delayed by 21 days. Investigators followed all study participants for 84 days to assess whether vaccinated subjects were protected against Ebola virus infection. The primary endpoint being laboratory-confirmed Ebola virus disease with onset of symptoms at least ten days after randomization, based on the incubation period for Ebola being on average ten days.
A total of 75 laboratory-confirmed cases of Ebola virus disease were identified in the 90 randomized clusters during the study period, of whom 33 patients died.
In the ‘immediate’ vaccination rings, nine people developed Ebola disease before ten days and none were reported after ten days. In fact those nine people developed disease within six days of vaccination with some developing symptoms within one day of vaccination. In the ‘delayed’ vaccination rings there were 16 cases of Ebola before the ten day period and 16 cases after the ten day period.
“There are sound scientific arguments suggesting that the vaccine itself may have altered the incubation period for Ebola – making it shorter than normal and allowing Ebola symptoms to emerge earlier than normal."-Dr. Vanden Bossche
All of the Ebola cases that were diagnosed in vaccinees occurred shortly (i.e., within max 6 days) after vaccination regardless of whether the vaccination was immediate or delayed. This observation is strongly supportive of the scientific plausibility that inflammation inherently associated with vaccination with a live replicating vaccine is likely to enhance the life-threatening immune inflammatory events known to be triggered by Ebola virus.
“In other words, those who got Ebola within 10 days of vaccination could have had earlier and more severe symptoms due to interference of the vaccine with the early, inflammatory stage of their immune response to the virus. If this were true, one might expect a greater proportion of deaths in these cases.”-Dr. Vanden Bossche
In fact, the case-fatality rate was 52% (15/29) in the immediate vaccination rings and 39% (18/46) in the delayed vaccination rings.
In this case, ring vaccination with a live virus vaccines, rVSV-ZEBOV, dramatically increased the probability of a lethal outcome in people who were vaccinated while already incubating the disease.
CONCLUSIONS: While Ebola virus infection is more severe than measles virus infection, this trial highlights potential serious issues with the practice of using vaccines as post-exposure prophylaxis. The effectiveness of PEP can be limited by factors such as the intensity and duration of exposure, and the timing of prophylaxis administration. Postexposure prophylaxis does not appear to be effective in settings with intense, prolonged, close contact, such as households and smaller childcare facilities. There are still many unanswered questions about the use of vaccines in this context, including the rationale behind this practice.
How does this practice affect the short-term immune response? Are antibodies generated? If so, are they protective?
How does this practice affect the memory response by giving the vaccine during infection?
Have systemic pro-inflammatory cytokines been measured in serum from vaccinated and nonvaccinated cases?
What is the presumed mechanism of protection with post-exposure vaccination?
Can the vaccine accelerate the emergence of disease?
Can the vaccine have a detrimental effect on the development of the disease?
Without understanding how long immunity lasts, there is no solid rationale for using any vaccine in a prophylactic setting. Until appropriate studies are conducted in animal models to assess this practice, vaccinating healthy individuals at risk of exposure lacks justification, as it could unnecessarily put them in harm's way.




POST 💰 EXPOSURE 💰 PROPHYLACTICS 💰Everybody get some 💰💰💰💰💰💰
Was anaphylaxis involved? Was this malpractice?