When Facts Became Dangerous: COVID and the Death of Honest Debate
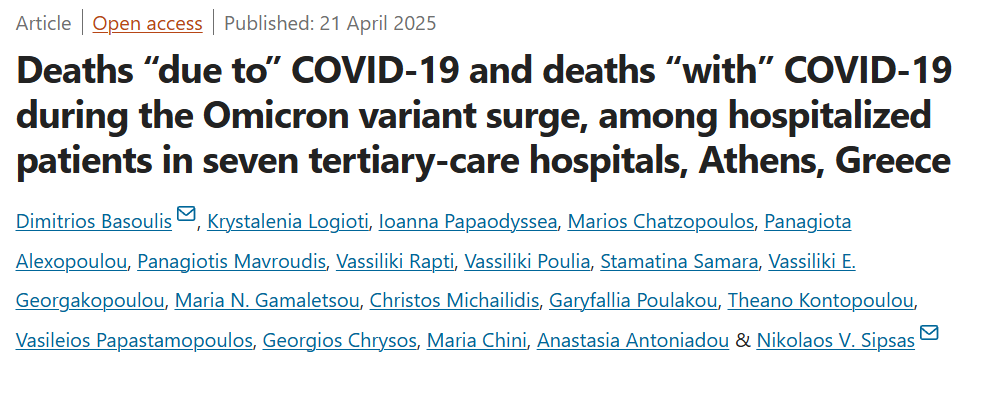
Study Confirms at Least 45 Percent of Listed “Covid deaths” Were Misclassified
I have been thinking a lot about this study since I posted it in a note and the more I think about it, the angrier I get.
The four-year anniversary of my dismissal from the Hawaii Department of Health is approaching. I was effectively terminated for exposing this very thing, the fraudulent misclassification of deaths as COVID-related. Despite the accuracy of my concerns, the truth seemed secondary to maintaining the prevailing narrative — and I was treated as a threat for challenging it.
I shared my thoughts on the matter shortly before heading to Hawaii for the hearing.
Heading off to Hawaii for the Arbitration Hearing
In August of 2020 I blew the whistle on the lies and COVID corruption in Hawaii. This was swiftly followed by retaliation and subsequent removal from my position.
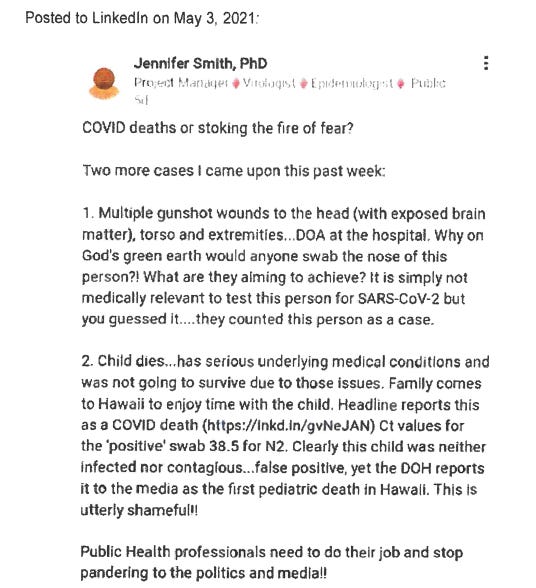
In short, Hawaii Department of Health leadership cited social media as the justification to discharge me from my position in May 2021, specifically this post:
In this LinkedIn post, I raised concerns about the misclassification of deaths as being due to COVID when they were not actually caused by the virus. I didn’t need a peer-reviewed journal to recognize that the data was being distorted but as more time has passed more and more of what I have said is being proven to be correct.
A new study has confirmed that at least 45 percent of listed “Covid deaths” were misclassified.
Researchers have pointed out an information bias related to case and mortality definitions for COVID-19, that varied among studies and sometimes within studies. Accuracy in defining the cause of death during the COVID-19 pandemic was of paramount importance for surveillance and intervention purposes.
In the UK, Denmark, and other countries all deaths, for which a positive SARS-CoV-2 PCR test was recorded within the 30 days prior to the date of death, were registered as COVID-19 deaths. Similar death coding practices were employed across most Western nations therefore, it is likely that death counts were artificially inflated to a comparable degree elsewhere.
In the US the Council for State and Territorial Epidemiologists definition was, “A person whose death certificate lists COVID-19 disease or SARS-CoV-2 or an equivalent term as an underlying cause of death or a significant condition contributing to death.” Thus a death could be classified as a COVID death even without a confirmatory laboratory test.
Therefore, throughout the pandemic, the above definitions were not able to determine accurately who died ‘from’ or ‘with’ COVID-19.
A team of top Greek researchers analyzed the death data from seven hospitals in Athens, Greece.
Among 530 in-hospital deaths, registered as COVID-19 deaths, in seven hospitals in Athens during the Omicron wave, 240 (45.28%) were reassessed as not directly attributable to COVID-19.
Those patients had died from other causes, but their deaths were recorded as being caused by COVID-19. Interestingly, patients infected during hospitalization were significantly more likely to be misclassified as COVID-19 deaths (OR: 2.3, p = 0.001).
There is a distinct difference between COVID-19 mortality and deaths “due to” COVID-19, where SARS-CoV-2 infection was the direct cause of death or triggered a series of events that ultimately led to death, from deaths “with” COVID-19, when the SARS-CoV-2 infection had nothing to do with the fatal outcome.
Death certification errors are common and range from minor to severe.
A comprehensive forensic audit of the deaths that occurred throughout the pandemic is essential in order to ensure the accuracy and integrity of the data used to inform public health decisions. Such an audit would provide transparency, helping to clarify the true impact of COVID-19 on public health, and address concerns about misclassifications or potential discrepancies. By thoroughly examining the circumstances surrounding these deaths, we can ensure that going forward policies are based on reliable information and that accountability is upheld in the face of one of the most challenging public health crises in modern history.
The death certificate is a legal document with diverse and far-reaching applications. It is the final certification of a patient's life and cause of death (disease or injury), provides invaluable information to the decedent's family, and is required for most end-of-life legal matters such as life insurance and inheritance. It also contains epidemiologic data that are essential for formulating vital statistics and allocating public health resources.
Given the importance of this document, it is crucial that its completion be thorough and accurate.
Unfortunately, errors in death certification are common and range from incomplete certificates and illegible handwriting to inaccurate causes and manners of death.
A study from twenty years ago was undertaken to determine the frequency and type of errors by non-pathologist physicians at a university-affiliated medical center in Vermont. Of the 50 clinician-certified death certificates reviewed for this study, 48 (96%) contained some degree of error.
Of the 50 death certificates reviewed, grade I, II, and III errors were noted in 72%, 32%, and 30%, respectively. Seventeen certificates (34%) had grade IV errors (wrong cause or manner of death). Multiple errors were identified in 82% of the death certificates reviewed.
Source: Table 1. Scale for Grading Errors in Clinician Death Certification
In another study, errors were found in 36 (37%) of the 98 death certificates analyzed. The most prevalent type of error was the use of a nonspecific diagnosis as the underlying cause of death (22 of 36 errors, 61%).
When there are preexisting comorbities it can be difficult to decide on the cause of death. These deaths usually require investigation by the office of the chief medical examiner or coroner to make this determination.
There are three sections on a death certificate: underlying cause of death (the disease or injury that initiated the chain of morbid events that led directly and inevitably to death), contributing cause of death (other significant diseases, conditions, or injuries that contributed to death but which did not result in the underlying cause of death) and immediate cause of death (the final disease, injury, or complication directly causing death) for reporting a chain of events leading directly to death.
For example, for a person who has hypertension and coronary artery disease but dies of metastatic colon cancer the cause of death would not be heart disease nor would those underlying conditions be considered as contributing factors. However, for someone who dies of a myocardial infarction (heart attack), those underlying conditions would be significant contributing factors to the cause of death.
In addition to major missed comorbidities, the grade III error category included major missed components of the cause-of-death sequence (immediate or intermediate causes); in other words, an important part of the “story” was missing. For example, listing adenocarcinoma of the colon as the cause of death without mentioning that the patient had died following partial colectomy, complicated by recurrent pulmonary emboli and lung infarction, is omitting a major portion of the patient's course.
If an individual with a pre-existing condition, such as liver cancer, passed away due to liver failure, yet tested positive for SARS-CoV-2 thirty days prior, how can this be justifiably classified as a COVID-related death? Such cases raise important questions about the accuracy of death classification and the potential for misattribution, which can significantly skew public health data and policy.
To revisit my LinkedIn post from 2021: An individual who suffered a fatal gunshot wound and subsequently tested positive for SARS-CoV-2 upon arrival at a medical facility should not be presumed to have died 'from' or even 'with' COVID-19.
CONCLUSION:
During the height of the pandemic, when fear and uncertainty were widespread, it was imperative for leaders, institutions, and individuals to uphold an unwavering commitment to truth in order to maintain public trust and support informed decision-making. Ensuring accuracy was vital at every stage — from classifying individuals as confirmed COVID-19 cases to determining whether deaths were truly attributable to the virus — as these determinations directly impacted the integrity of public health data, shaped societal understanding of the crisis, and influenced the formulation of effective and appropriate policy responses.
Yet in many instances, those who raised legitimate concerns about data integrity, policy inconsistencies, or potential fraud were met not with dialogue but with hostility. Vilifying and terminating individuals for exposing potential fraud or challenging misinformation was not only a grave injustice to those individuals, but also a dangerous suppression of accountability that undermined institutional trust, stifled open discourse, and set a troubling precedent for the treatment of dissent in times of crisis.
My experience has only strengthened my belief in the importance of accountability and the courage to stand for what is right, even when faced with tremendous opposition.







Knowing the true cause of death would help a lot to determine what really caused the massive increase in all-cause deaths in 2020-2022 in the US. There were several unprecedented death waves in the US in 2020, the likes of which haven't been seen since Spanish flu. Simply attributing them to "Covid 19" doesn't really tell us anything--it looks like mass-murder more than anything.
I hope one day when the time is right that you sue the Hawaiian authorities for damages